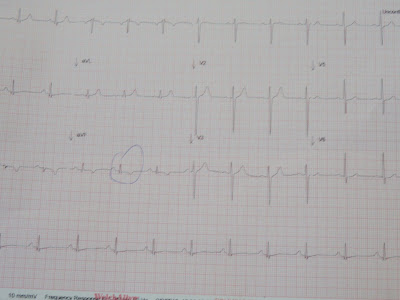
So I get a call from one of the ANA docs asking me to see a pt. He states he is a young guy with tachycardia and it won't go away, so he wants my help. A month or two ago, we had a young guy with AVNRT(arrhythmia), so I was thinking it was something like that. When I show up I could tell this was not going to be what I was expecting. There is a 24 y/o male in obvious respiratory distress, pulse oxygenation (little thing that goes on your finger) is 88% on a face mask (not good) and his heart rate is 120. The doc states he is treating him for pneumonia for the past 36 hours (it was a three day holiday weekend), and tries to communicates that also in his differential diagnosis is pulmonary edema(fluid in the lungs) and pulmonary embolism (clot in the pulmonary arteries). I was a little confused because I thought he was trying to communicate that the patient was getting better, ie: his heart rate was now only 120, and it was 180 the day prior, his hypoxia and respiratory status are better. The patient told me he felt better too. So I look at his chest xray, which was not that bad, and if I looked hard, could kinda see a pneumonia, but nothing overt that could explain his hypoxia (low oxygenation). I also look at his EKG because after all, the whole reason he called me in was for tachycardia. There is an incomplete RBBB, and some other "odd" changes, but at first I wasn't sure why, I just knew things didn't add up. So I asked the pt why he came in, he said, I have been short of breath for 6 days, coughing up small amounts of blood and I passed out the day I came in. As soon as he mentioned the blood and passing out I knew it was going to be something bad. I listen to his lungs and they were unfortunately clear... I knew immediately he had a pulmonary embolism. I look at his legs and the right one is red and swollen. We immediately treated him with lovenox. We decided not use thrombolytics (tears up the clot in his lung) because his blood pressure was stable and once we sat him up, his oxygen sat came up to low 90s. The patient did well for the first 10 days, came off oxygen, heart rate in the 80s.....until very early one morning he decided to get up and walk to the bathroom, which we had warned him not too do, and he passed out. I get woken up to come to the hospital, but they coded him for about 20 or 30 minutes and he was dead by the time I got there. I told them not to feel bad, there was nothing they could have done.
In hind-sight, the interesting thing about his EKG is that he had an S wave in lead I, Q in lead III and abnormal T wave in III, which fits the classic but rarely seen EKG pattern for pulmonary embolism.